High cholesterol? There's a bug for that.
Deep in the uncultivated wilds of the microbiome, there's a natural solution for one of the biggest drivers of heart disease.
A few years ago, I got a call from my doctor the day after a physical. The labs were back and everything looked good, he said.
“…and your cholesterol is amazing, even for a young man. What do you do? Do you avoid meat, eggs?”
“Uhh, no, I eat a fuckton of eggs,” I said.
He gave a sort of verbal shrug, and said something about good genes before we hung up. Maybe he was right—but I don’t think they’re human genes.
See, the metabolism of cholesterol and its derivatives is one of the first places where scientists began to recognize the importance of the microbiome—that gut bacteria can have an impact on our health far beyond the GI tract.
The Basics
First things first: not only is trying to cut cholesterol out of your diet a culinary bummer, it doesn’t even do that much good. Unless you’re on a four-eggs-a-day kind of regimen, your own liver—not your diet—is the main source of cholesterol in your body. It makes it from scratch. But since high blood cholesterol is linked to heart disease, cholesterol-lowering meds like statins (which block cholesterol production in the liver) are some of the most heavily prescribed drugs in the world today.
Your liver is making cholesterol for a reason, though: it’s not just there to clog up your arteries. It helps cell membranes keep the right blend of flexibility and rigidity, and acts as a kind of detergent in the GI tract, to help you absorb fats from the diet.
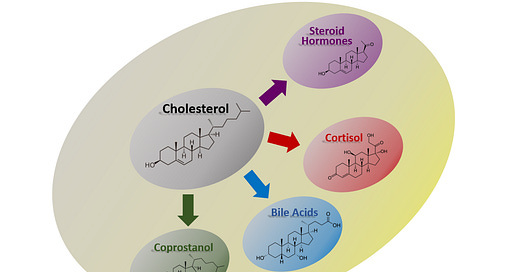
It’s also the basic chemical structure that the body uses to create steroid hormones, like testosterone and the estrogens—the word steroid comes from sterol, as in chole-sterol. Cortisol and corticosterone, the body’s major “stress” hormones, are cholesterol derivatives. So are bile acids, which are secreted into the intestine along with cholesterol to help dissolve food and regulate intestinal pH.

All these cholesterol derivatives (except cortisol) share an important property: They don’t just circulate in the bloodstream, they cycle through your GI tract.
When you’re not eating, cholesterol and bile acids from your liver build up in a little sack underneath it—the gallbladder. The mixture they form is bile. Bile is a little bit of biological magic, in that it bends the rule that oil and water don’t play nice together. When you eat, the gallbladder dumps bile into the gut, and these molecules ride the waterslide all the way to the end of your small intestine, dispersing fat into digestible micro-droplets along the way. As those fats are absorbed into the bloodstream, most of the cholesterol and bile acids are too. They’re carried back up to the liver, which sorts them back out toward the gallbladder, and the whole process—called entero-hepatic recirculation—can repeat.
(An aside: activation of your bitter taste buds stimulates the production of bile in the liver. This is part of why digestif drinks are often bitter, and it’s why the most offensive-tasting herb in my apothecary cabinet is also one of the most potent liver and digestive tonics.1 This is largely unrelated to the main point, but I feel it’s important to mention because it's a good reminder that your tongue isn't just for telling you whether something is food or not: the act of tasting a food kickstarts the digestion process by providing information about its chemical makeup, and your digestive system reacts accordingly, warming up the right machinery to handle that thing. For instance, it's been shown that chewing a piece of pie can spike your insulin levels, even if you don’t swallow any. This seems like it has implications all its own, but those are beyond the scope of this post.)
Anyway…
The body is thrifty. An individual molecule of cholesterol might pass out into the GI tract, get absorbed into the blood, and then go back to the liver seven or eight times over the course of a single digestive cycle. And on each pass through the gut lumen, there’s potential for bacteria to get their hands on it. When they do, certain species can turn it into a molecule called coprostanol.
It’s an itty bitty chemical change, so small that it’s hard to even spot: a hydrogen atom introduced, a double-bond turned to a single bond. But this makes a huge difference in terms of its chemical properties.
See, coprostanol isn’t soluble the way cholesterol is. That means that, when cholesterol gets converted to coprostanol in the GI tract, it can’t be reabsorbed into the bloodstream—it stays put in the GI tract until it leaves the body as part of a poop. It’s out of the game.
As you might expect, this can substantially lower your cholesterol levels.
Only certain species of bacteria can perform this reaction, and they’re not well-characterized, existing largely in the “unculturable” wilds of the microbiome—but they’re apparently common enough that most people (and other animals) excrete some amount of coprostanol in their stool. But the composition of your microbiome determines how much of your cholesterol gets “deactivated” by this process, varying wildly across the population. In some people, it’s less than 5%. In others, it’s more than 90%.
In a massive 2005 study exploring the subject, researchers found a striking pattern in the data around how much coprostanol people’s microbiomes produce: Roughly 17% of young men had such low levels in the stool that they were classified as “non-converters”. Among elderly men, on the other hand, only 2% fell into this category.
Why the discrepancy? How can we explain that 98% of elderly men have cholesterol-reducing2 gut bacteria, but only 83% of young men do? What’s happening to the other 15% of young men?
There’s two main possibilities. Either:
They’re gaining the ability to convert cholesterol to coprostanol at some point, or…
Dying before they make it into the “elderly” cohort.
Researchers seem to think it’s the latter.
This makes good sense to me. Your liver is constantly churning the stuff out, and you’re eating it too. Judging by the fact that nearly all other mammals have the cholesterol→ coprostanol pathway in their microbiomes, these bacteria have probably been with us for most of our evolutionary history, and we’ve entrusted them with the task of ensuring that cholesterol doesn’t build up to artery-clogging levels. They hold up their end of the bargain, as long as they’re able—but if you hit them with antibiotics…well, sorry pal, you’re on your own, maybe permanently.
As a bonus, coprostanol production is unusually low in families with a high risk of colon cancer, suggesting that heart disease isn’t the only thing it’s involved in—although this might just be a common-cause correlation, because if antibiotics have deleted the coprostanol production genes from your microbiome, they’ve probably taken a few other important features along with them.
But imagine what an extraordinary future we could have: one where, if you’ve got high cholesterol, you could solve the problem with a single dose of the right probiotic. It’s practically sci-fi tech: a microscopic machine that sits in your gut and keeps you healthy by transforming cholesterol into this harmless byproduct. Self-replicating, and drawing the energy it needs from the food you were eating anyway. It’s beyond anything we could create right now—but it already exists, ready-made to work inside the human body, fine-tuned over millions of years of evolution.
For some reason, folks hate it when I bring up a finding with great implications for human health, and then go straight to pontificating about it Carl Sagan-style without stopping to tell them how to avoid being in the 15% of people whose microbiomes doom them to die young. Oftentimes, this is a bit of sleight of hand, because I’m not really sure how, aside from “find someone with [trait X] and eat their poop”.3
If you don’t have any of the right species in your gut, there's not much else you can do for now. This is one of the hundreds of biochemical functions in a healthy microbiome that no existing probiotic can perform. But if you’re at the lower-activity end of the “cholesterol reducer” spectrum and you want to encourage the right bugs, I have a clue. There’s a paper in the literature, reporting that the bacteria which produce coprostanol rely on plasmalogens—a type of phospholipid found in lecithins. You find lecithins in lots of foods, often as an additive to help things like chocolate blend smoothly.
I don’t trust soy lecithin for reasons explored in The Thousand Secret Ways the Food is Poison, and I think it’s generally best to get foods in as close to their unrefined state as possible. Shellfish like mussels are high in plasmalogens, but so are—ironically enough—eggs.
Funny, isn’t it? One of the highest-cholesterol foods out there also has a good dose of the molecular fuel that helps your microbes handle it in a healthy way. Honestly, I’m willing to take it a step further and say: Maybe the real solution for high cholesterol is to eat more cholesterol.4
It’s counterintuitive at first, but this kind of dynamic is common in the gut: If you’ve got an overgrowth of Candida or some other fungus, one of the best things you can do is to eat more mushrooms. Fight fire with fire, and fungus with fungus—because when you eat a mushroom, you’re feeding bacteria that love to eat fungi. They proliferate, and once the mushroom you ate has passed on, they go looking for something else fungal to snack on, and help control the Candida. This is what I mean when I tell people that, if you want to understand the human body, you must take the ecological perspective.
Microbiome science suggests a new twist on an old saying. It’s not “You are what you eat”, but “You are what eats what you eat”.
I’m not sure if this is tautological, or deep, or both.
🖖🏼💩
Friends have compared it to that potion Dumbledore has to drink in Half-Blood Prince.
Here, the word “reduced” applies in both its meanings. The chemical conversion from cholesterol to coprostanol is a reduction reaction, i.e. the opposite of oxidation. The fact that, when this reduction happens in your GI tract, it reduces the overall level of cholesterol in your blood is a convenient coincidence.
Email for a DIY FMT protocol.
Here, as everywhere, the quality of food is important. Eggs laced with coccidiostats and tryptophan synthesis inhibitors probably don’t lend themselves to bacterial transformation the same way organic eggs do.




Does this mean, if you eat meat, you will encourage meat eating bacteria, because when they run out of meat they will start looking for meat to eat and because we are made of meat they will start eating us?
Fascinating!